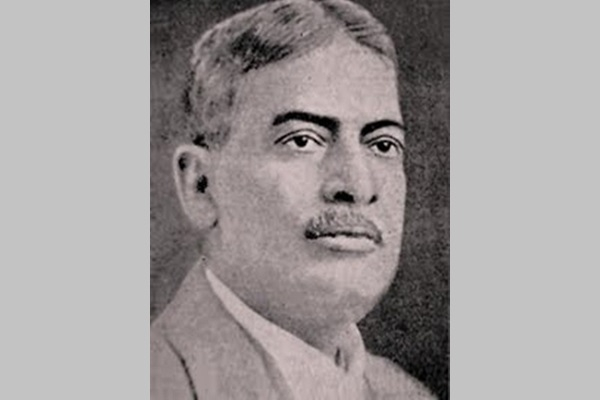
Brahmachari: The Forgotten Saint Of Calcutta
- This is the story of a forgotten genius of Indian science who saved millions of lives but went unrecognised by both government and people.
The gleaners spread around, and here and there,
Spike after spike, their sparing harvest pick.
The story of Upendranath Brahmachari is the story of a forgotten man, remembered only when a street in Kolkata that bears his name shows up on Google Maps. Even here, Brahmachari was handed down a recognition that for more than a century belonged to John Claudius Loudon, the Scottish botanist. A nation that knows not how to honour its living, knows not how to honour its dead.
“Brahmachari was a genius but a maverick; a rebel,” remarked once the late Asima Chatterjee, an alumni, like Brahmachari, of Calcutta University, and a genius in her own right, having made pioneering contributions to Alkaloid and Natural Products research. “This was the thirties we are talking about. The nation was in the grip of Nehru and Jinnah and Patel and Mahatma Gandhi. But for me, there was one other Mahatma, who no one really knew, leave alone worship. No one except us, the students of Calcutta University. Thakurda we called him. He was a legend, someone who had beaten Ronald Ross, no less. But an eccentric legend. His quirkiness was the stuff of folklore. One day something snapped in him. He protested against, of all things, the hand-drawn rickshaw. “We want independence but are fine with a man pulling another man?” he cried. The very next day we saw him come in a rickshaw. Except that it was empty of passengers and he was pulling it. Imagine. There ensued mayhem. The English professors were aghast. Unconcerned, Thakurda, as always in his pristine kurta and dhoti, brought the rickshaw to a halt, dropped the handlebar coop and hopped out of it, then strolled calmly into his lab. I can’t forget the scandal it caused. Yes, he was the Mahatma India forgot.”
Mahatma or not, Brahmachari was nominated multiple times for the Nobel Prize. Like Gandhi, he never got it. But unlike Gandhi, he didn’t make it to our currency notes. There is no holiday or a dry day to celebrate his birth or death anniversary. There is no stamp minted in his name. There are no political parties that sing his paeans, no government schemes that are burdened with his legacy. He exists only in sunset memories of the few who knew him, and of the even fewer who come across his name accidentally while consulting Google Maps on their smartphones or spending lazy afternoons on the internet. His story is, in a strange, sad way, the story of our nation. It is the story of tea, triumph and tragedy. And because every great story has a prologue, written for it by fate, one that tethers its soul to history, this one is no exception.
The year is 1815. Great Britain has emerged victorious in the Napoleonic wars, and with the simultaneous crumbling of the Spanish empire, the excitement of the cash-strapped Britons, eager to hunt for opportunities to invest in the new world, has reached fever pitch. The new world is Latin America, with its freshly minted independent countries, all erstwhile colonies of Spain. Flourishing on conceit, arrogance and an active debt-bond market, London has become the financial hub of Europe, delirious with untold riches and wholly unaware of meeting its own Waterloo just 10 years hence.
The year is now 1825. Many of the new-world enterprises and governments have defaulted on their borrowings. Panic has taken hold in both the new and old worlds, heralding the first emerging markets’ financial crisis. The Bank of England has jumped in to bail out banks and independent investors, but the damage is beyond repair. The stock market has crashed, with catastrophic implications for the blue-chip stock – that of the East India Company. The company has come under the scanner for its monopoly over the tea trade, which has cost the rich people of Great Britain in excess of two million pounds sterling. The horror and hurt to the pride of this tea-loving nation is further compounded by the fact that they are left behind by the poor people of Australia, who are procuring tea directly from China. To rub salt into the wounds, the Aussies are savouring tea at much lower prices. Just not cricket.
Meanwhile, the eastern-most part of the British Empire is at war. Her subjects, the Indians, are fighting simultaneously on two fronts: against deadly diseases, and, for the British army, to annex the principalities of Assam and Manipur from Burma. Bengal has turned into the delta of death – 150,000 men of the Bengal regiment engaged in the first Anglo-Burmese war, fighting incessant rain and dangerous terrain, are dead. The port city of Jessore (now in present-day Bangladesh), the jewel in the crown of Pratapaditya, the king who fought against the Mughals the famed tactical battle of Salka, has come under the dark throes of an incurable epidemic called “kala-azar” or black fever. It has claimed no less than 75,000 lives. Jessore has turned into a graveyard once more.
Meanwhile, the British Indian army has tasted victory in the Anglo-Burmese war, a taste soured by a whopping war bill of thirteen million pounds sterling, worsening further the economic crisis plaguing the Old Blighty. It doesn’t take long for this crisis to engulf India in its snarl. The chattering English classes have begun to chatter. Eyebrows are raised over the special privileges granted to the East India Company. Why should British military and naval services continue to protect a trading company? How could these tea dealers act as sovereigns? Who is paying for all this?
The lords convene, acting on behalf of the crown. With the idea to grant itself time and focus to keep India on the leash, the British Parliament dismisses the Company’s monopolistic tea trading rights with China. The Company is devastated. No one likes a blow to their ledger, not in the least the lordly grocers of Leadenhall Street. Thus begins the quest to discover a new diamond, a quest that would alter the world forever.
To fill up its depleted coffers, the Company decides to turn the newly annexed region of Assam into a vast tea estate. The chaas-drinking natives would have to be proselytised into chai-drinking ones, and at the click of one’s fingers, as though by magic, would materialise a giant captive market.
Charles Alexander Bruce, the man who led bravely in the Anglo-Burmese war, is charged with altering the topography, demography and drinking habits of Assam. His sole mission is to ensure that the Company’s accounts rise and shine once again. This marks for India the beginning of a new era – that of a plantation economy. The Company’s search for a new diamond has ended. It is tea.
Bruce gets to work. As an essential trade requirement, access to the region is opened. Connections via road and steamer services to Bengal enable rapid movement of people and supplies. The gates to El Dorado have been unlocked. In consort, and unknown, quietly slithers in an unwanted devil, kala-azar.
In quick time, the wild wastelands of Assam are transformed into sprawling estates of manicured greens. Matching this progress, proceeding from village to village, from Jessore via Nadia through Hooghly, kala-azar casts its deathly shadow over Bengal, garbed as Old Burdwan fever. Next, and it was only a matter of time, it hurls into the Brahmaputra valley to reach up to the Garo Hills. The year is 1870.
District after district in the Brahmaputra valley is decimated by this unexplained fever, a “fever of malarial poisoning that darkens the skin in its chronic form”, as explained in his Sanitary Reports on Assam by Captain Clarke McNaught, Civil Surgeon of Tura, the district HQ of Garo Hills. Kala-azar has dug its fangs in the local population, lacerated already by the socio-cultural, political and economic chaos brought about by the repeated Burmese incursions by the British. They hold them responsible for its emergence and spread, calling it the sarkari bimari. It doesn’t take long for the Garos to figure out that the only way to escape the scourge is to leave the infected and diseased villages and be on the move constantly. As a result, vast swathes of inhabited lands have become severely depopulated. The few who are fortunate enough to survive the black fever onslaught have turned bitterly recalcitrant towards the British, refusing to serve in the tea estates. Mutiny beckons. The much-vaunted plantation economy is about to collapse.
Hit by an acute shortage of plantation workers, the British induct “Arkutti agents” or “coolie catchers” to source cheap labour from areas such as the Chhota Nagpur. Brought over false promises, paid too little, fed too less and thronging in unhygienic conditions, large numbers of hired coolies fall victim to disease and death. The medico-social problem of kala-azar, a creation of the plantation economy itself, is now threatening to engulf all who dare to come in its way. No one, from agents to migrant labour to locals to even the masters, no one is spared.
The sarkari bimari, of no importance or worry to the Sarkar until now, has become a matter of grave concern, enough for the British to call for urgent measures to tackle it. The mutiny must be quelled, the revenue registers must be kept ringing, the tea business must be salvaged. The black diamond cannot be allowed to turn into Black Death, or the many names it has come to be known by: sarkari bimari (Garos), kala-dukh (Purnea), kala-jwar (Darjeeling), pushkara (Jalpaiguri), dum dum fever (Calcutta), sahib’s disease (Assam). The mortality rate is an incredible 90 per cent. It appears that nothing can save the east from being ravaged by this curse.
But the luck turns. And so does tense.
1873. Those were troubled times, days of devastation for Assam and Bengal, when Upendranath was born. Villages resounded with wails and lamentations of those whose spirits had been broken, and fields were strewn with skulls and bones of those whose spirits had escaped.
Born in Jamalpore, in the Monghyr district of Bihar, Upendra’s father, Dr Nilmony Brahmachari, was a highly respected medical practitioner, and a household name in both European and Indian communities. Upendra loved mathematics from childhood. With an illustrious academic record at school, decorated with double Honours at graduate level in Mathematics and Chemistry from the Presidency College, one would have thought he would continue in the field. But how could an educated, conscientious man stay unaffected by the misery all around him?
Upendra set out to be a polymath. He chose to learn medicine and surgery next, following in his father’s footsteps. Once again, he stood first in the course, joining the Provincial Medical Service in 1899. By 1902, he had earned his MD from Calcutta University, alongside a PhD in physiology – a rare distinction. That he was to achieve something even more remarkable in the coming years had not yet dawned on him.
His diligence in research and teaching, and dutiful commitment to medicine earned him appointments at the medical schools in Dacca and Calcutta. His fame was beginning to spread. Soon, he was appointed as Additional Physician at the Calcutta Medical College – one of only two Indian doctors outside of the Indian Medical Service (IMS) cadre to have ever been inducted. All positions at medical schools were, until then, exclusively held by doctors of European origin, selected and trained in England to serve in the IMS.
Meanwhile, another polymath and a man of medicine, Major Ronald Ross, an officer with the IMS in the Madras presidency, had successfully uncovered the culprit behind a seemingly insurmountable health challenge: Malaria. A spectacular discovery, that of the malarial parasite and its life cycle, earned him the 1902 Nobel Prize in Medicine. In keeping with the prevailing view that kala-azar could be a form of cachexic malaria, and disregarding Sir Ronald’s unwillingness to extend his stay in India, the panic-ridden British government appointed him in charge of the newly instated Kala-azar Commission. His posting orders for Darjeeling followed. Reluctant to accept the assignment, he remarked: “Columbus having sighted America was ordered off to discover the North Pole.” Unsurprisingly, his disinterest in the appointment, coupled with his longing for horrible weather and baked beans, meant he couldn’t make the scientific breakthrough the crown had hoped for, except that his eye for detail and meticulous record-keeping resulted in capturing patient case histories from the districts of Nowgong and Naxalbari, which had witnessed a third of their population wiped out because of kala-azar.
Based on Sir Ronald’s record of observations from 1899, his guide and mentor Dr Mason suggested kala-azar could well be different from Malaria, more so as it was unresponsive to quinine even in large doses. Confirmation of this startling postulate came a year later, through Major W B Leishman, a professor of pathology at the Royal Army Medical College, London. Leishman discovered peculiar bodies in the spleen of a soldier who had died of dum dum fever at Netley Hospital, Calcutta. These appeared nothing like the malarial parasite. Leishman suspected them to be of the trypanosome family, similar to the parasites that were decimating most of The Gambia through sleeping sickness.
News of the discovery spread like wildfire. Similar spleen bodies were reported by professor Charles Donovan of Madras Medical College, in patients suffering from prolonged fever and spleen enlargement. In 1903, Donovan confirmed that this parasite was different, certainly not a trypanosome, and never seen or reported before. The parasite was christened Leishmania donovani – harbinger of the deadly kala-azar. By 1904, Sir Leonard Rogers of The Royal Society of Tropical Medicine and Hygiene could cultivate the parasite in lab cultures and demonstrate its flagellated form. News of the same parasite being observed in patients from places such as Ceylon, Central China and the Mediterranean coast (Sicily, Greece, Tunis, Tripoli, Portugal) indicated that the disease was not uncommon or geographically isolated, its prevalence correlating strongly with tropical weather.
With the miscreant’s identity now out in the open, the conquest of kala-azar commenced. It had two broad objectives. What, or who, transmitted the parasite into humans, and which compound could serve as an antidote for it. It was the second objective that kindled young Upendranath’s curiosity. Simultaneously, many of his medical contemporaries in and around Calcutta decided to tackle the first. The race to beat black fever had well and truly begun.
Upendranath, meanwhile, had made quite a name for himself in Dacca as a young physician of great merit. But despite a flourishing practice, his heart ached for research and discovery, prompting him to move to Calcutta, where he accepted a teaching position at Campbell Medical College. The year was 1905; a special year or, as it would later be called, Annus mirabilis. Koch had won the Nobel Prize, Bose was perfecting his electromagnetic detector, Haber had invented his process, Freud had expounded his theories on sexuality, and there was this young, impertinent patent office clerk by the name of Einstein who had explained, in one go, Brownian motion, photoelectric effect, special theory of relativity and mass-energy equivalence.
If the year was special, so was the city. The Calcutta of those days carried an air of modernity mixed with tradition. It was brimming with philosophers, followers of the Brahmo Samaj and prolific thinkers from the fields of science, art and literature. The Bengal Renaissance was at its helm. J C Bose, Rabindranath Tagore, Sukumar Ray, among many others, were pushing India’s foray into empiricism, experimentalism and modernity.
For Brahmachari, modernity would have to wait. Working in a dingy room the width of a dozen coffins, he threw himself into finding a cure for kala-azar. His lab, if it could be called that, had no running tap or electricity or a gas point, but this did not seem to bother him in the least. He had one job.
And he got it done.
Brahmachari’s deep interest in chemistry drew him to the nascent field of chemotherapy or pharmaco-therapeutics – that is, treatment of a disease with chemical compounds. By 1904, Paul Ehrlich in Germany had established a proof of principle by using trypan red, a synthetic dye, to kill the parasites that caused sleeping sickness. The concept, of testing heavy metals as drug candidates, had not even reached the neighbouring countries in Europe, when Brahmachari began planning and setting up experiments in his primitive lab in Calcutta.
Meanwhile, doctors from Brazil and Italy reported positive treatment results for infantile kala-azar with a derivative of antimony – antimonyl potassium tartrate, commonly known as tartar emetic. Brahmachari knew already of Dr Leonard Rogers’ limited success with administering antimony to treat 10 kala-azar patients in India. He now saw a ray of hope. But it was brief and short-lived. A tediously long and painful regimen, not to mention the alarmingly high toxicity of tartar emetic, was undesirable as a treatment.
Through his clinical experience, Brahmachari was long aware of the curative properties of antimonial salts. Now he took it upon himself to discover less-toxic and easy-to-administer chemical compositions for treating kala-azar. Tartar emetic was not available in India in those days. He began devising methods for laboratory preparation of a pure colloidal form of metallic antimony. Toiling for months, he finally struck gold, or, to be sure, antimony, in the process also developing a special apparatus to administer metallic antimony intravenously. His novel method was published in the October 1916 issue of the journal ‘The Lancet’.
Meanwhile, in 1919, the Assam government approved the use of tartar emetic for kala-azar treatment. Available as a highly pure solid, it was to be injected as a 1 per cent solution, in increasing doses, and over a period of three months. Regulations were put in place under the Epidemic Diseases Act for patients to not exit before completing the entire course. But it was a non-starter. The programme was handicapped by rampant non-adherence, with patients dropping out of the three-month course at the slightest hint of improvement or because of appalling side-effects. Stocking the drug for long in rubber-capped flasks was another practical problem. Repeated puncturing of rubber caps to dispense periodic doses led to bacterial contamination of the drug in the tropical climate of Assam and Bengal. The effort failed. Kala-azar could not be reined in.
In the same year, Brahmachari won a support grant from the Indian Research Fund Association for his research on antimonial drug candidates. To avoid limitations presented by inorganic antimonial salts – those of storage and the terrible side-effects – he shifted focus on developing other combinations of antimony. Inspired by Ehrlich’s approach of combining arsenic metal with organic groups to produce less toxic compounds, Brahmachari attempted to design and synthesise organic antimonials (with antimony bonded to carbon), his over-arching aim being designing molecules that fulfilled Ehrlich’s criteria of therapeutic benefit – to achieve maximum ‘parasitotropism’ with minimum ‘organotropism’.
Time was running out. Millions of lives were at stake. Ever a team man, and known to be an encouraging and inspirational mentor to many, Brahmachari put together a squad of young and enthusiastic organic chemists from Calcutta University. Dozens of alternate antimonial preparations were synthesised and investigated, each one for its treatment effectiveness, route of administration, dosing protocol and toxicity.
The year 1922 is usually remembered as Banting’s year, in honour of Sir Frederick Banting (Nobel Prize, 1923), the Canadian doctor who accomplished the first successful treatment of diabetes with Insulin that he painstakingly isolated from fetal calf pancreas. The year also turned out to be Annus mirabilis for an equally unassuming and dedicated doctor toiling thousands of miles away.
One of the compounds in the list of dozens prepared by Brahmachari’s lab, urea stibamine (combination of urea with stibanilic acid), showed outstanding superiority over others in treating kala-azar. The first series of successful cases was published in October of 1922 in the Indian Journal of Medical Research, with results that were beyond expectations. In 1923, Major Shortt and his collaborator Dr Sen from the Pasteur Institute, Shillong, reported exceptional performance of the drug on kala-azar patients in Assam.
It was decidedly a miracle. What took upwards of 12 weeks to cure now took barely two, and without any discomfort or intolerance. Remarkably, as was soon discovered, there occurred no relapse. Urea stibamine could cure the most severe cases of fulminating kala-azar, even those resistant to tartar emetic. Beside themselves, Shortt and Sen wrote the following recommendation to the Indian Kala-azar Commission: “We consider that the value of urea stibamine has been established as the most efficient drug at present for the treatment of Indian Kala-azar. The conclusion is based not only on the experience gained in a series of cases, both Indian and European, which have passed through our hands or which have been treated with urea stibamine under our direction, a number totaling nearly one hundred cases.”
In urea stibamine, Brahmachari had found the Holy Grail any drug discoverer would wish for – shorter treatment regimen, stable compound, superior efficacy and low toxicity. Here it was, then, a tiny molecule, the result of the many torturous hours and days spent in a hot, dingy laboratory that he incidentally regarded as a place of pilgrimage. In his words, “I recall with joy that memorable night in the Calcutta Campbell Hospital at Sealdah, where after a very hard day’s work I found at about 10 o’clock that the results of my experiments were up to my expectations. But I didn’t know then that providence had put into my hands a wondrous thing and that this little thing would save the lives of millions of my fellowmen. I shall never forget that room where Urea Stibamine was discovered. The room where I had to labour for months without a gas point or a water tap and where I had to remain contented with an old kerosene lamp for my work at night. To me it will ever remain a place of pilgrimage where the first light of Urea Stibamine dawned upon my mind.”
Can one undertake a pilgrimage if the god is unknown? Can one call a room dingy if one does not notice the rising damp? For Brahmachari, just like for Banting, saving lives was all that mattered.
In the following weeks and months, urea stibamine became the gold standard treatment for kala-azar, backed by published papers that extolled of its remarkable performance in Badlipur, Solana and Hantley tea estates, and all the major medical colleges of Calcutta. For a disease that had been incurable for more than half a century, the discovery of urea stibamine was nothing less than a phenomenon. The kala-azar mortality rate plummeted to 10 per cent from a ghastly 90 per cent. Urea stibamine’s reputation as a wonder drug spread quickly to all parts of India. As Brahmachari, keeping true to his unassuming predicament, remarked in one of his papers from October 1924: “It is evident from an economic point of view, and in the interests of the miserable sufferers, that the use of urea stibamine in the early stages of the disease cannot be over-emphasised.”
Even as urea stibamine brought Brahmachari into prominence, he continued to make prodigious breakthroughs on kala-azar, and also popularise and spread the knowledge gleaned. Known to be a likeable and endearing person, the gatherings he would host for his British and Indian friends in his large house in Calcutta soon became fertile grounds for newer discoveries. “The fare was always good and the conversation even better. If all distinguished Indians, and for that matter all British officials, had shared his liberal outlook, many of the difficulties of India today would have been solved before they have time to develop,” said ‘The Lancet’, in his obituary (09 March 1946).
In 1922, the year he gave to the world urea stibamine, Brahmachari also discovered a new, deadly form of kala-azar. He called it Dermal Leishmanoid, marked by the appearance of sudden eruptions on the face of the patients without fever or other complaints. He observed it as a disease in partially cured cases of kala-azar, along with those who had no history of the disease at all. It was later renamed as Brahmachari’s Dermal Leishmaniasis.
Soon, heralding another major breakthrough, the transmitting vector for kala-azar was identified, solving at last the one remaining piece of the puzzle. The Indian Kala-azar Commission, which had been taken under the auspices of the Royal Society in 1924, confirmed sand-fly (Phlebotomas) as the carrier of Leishmania donovani, the causal parasite.
The following year, in 1925, the Assam government issued through its Health Bulletin a guidance drawn out by Major Morison (Director of Public Health, Assam) that treatment of all kala-azar patients be carried out using urea stibamine. It had detailed instructions on the dosing, preparation of the injectable solution, equipment and sterilisation requirements. In his concluding remarks, Major Morison said: “We find that 185,054 patients suffering from the disease have been treated, of which 166,545 would have undoubtedly died without proper treatment. The benefit conferred in Assam by this campaign against the disease can be estimated when it is realized that the treatment has converted the death rate of 90 percent into a recovery rate of the same percentage. We have good reasons to hope that we shall one day be successful in stamping the disease out of Assam.”
Morison was proven right. By 1932, close to half a million lives had been saved. The drug found ready and immediate acceptance in Greece, France and also in China.
As for what Brahmachari’s discovery did for tea production, the proof lay in the pudding. In 1879, London imported 70 per cent of its tea from China. By 1928, India had become the largest exporter with 39 per cent share, followed by Ceylon. Indians by then had also developed the taste, and the aspirational value that went along with it, of tea drinking. The domestic market in the 1920s was already valued at 50 million pounds. Consumption doubled in the 1930s. The black diamond had regained its shine.
In 1924, the British government conferred on Brahmachari the title of Raibahadur. A knighthood soon followed, to acknowledge his spectacular humanitarian contribution to society.
Raibahadur Sir Upendranath Brahmachari died on 6 February 1946. With him died the story of his colossal effort in saving millions of lives. The Indian government never conferred upon him a posthumous Padma award, any Padma award, leave alone a Bharat Ratna. A recent survey conducted by Probashi, a Bengali magazine, showed that seven out of 10 people had never heard the name Upendranath Brahmachari. Perhaps that is how Brahmachari would have preferred it. The difference between the great and the ordinary is simply this: that the ordinary think they are great and the great think they are ordinary.
As for kala-azar, it continues to be a menace, the second-biggest parasitic killer in the world. Strange are the quirks of fate in that, like Brahmachari, whose contributions and memory are neglected by the country of his birth, kala-azar is categorised officially under “Neglected Diseases”. Call it complacency or lack of funds, for almost three decades after Brahmachari’s death, further research on kala-azar was overlooked and ignored. Urea stibamine continued to be the gold standard in treating kala-azar. It was thought the scourge had been brought under control. But it re-emerged in 1977. Bihar was the first to succumb to it. Another salt of antimony, Sodium Antimony Glucamate (SAG), which was being used for treatment in the Mediterranean, was used to tackle the Bihar epidemic. It failed to deliver the desired results. Five strenuous years and intensive dosage studies conducted by Dr C P Thakur (who later became India’s health minister), a cure rate of 90 per cent was achieved. Since then, kala-azar continues to flare up periodically in India along with neighbouring Bangladesh and Nepal. Despite all efforts and availability of modern antibiotics, it remains endemic to 52 districts of Bihar, Uttar Pradesh, Jharkhand and West Bengal. Being the disease of the marginalised, kala-azar brings with it an enormous socio-economic burden. It remains untamed, affecting mostly the poorest of the poor, and especially the Musahurs, or rat-eaters, a Dalit community that is forced to live in unhygienic conditions.
The recent availability of complete genome sequences of multiple Leishmania strains would doubtless help gain more insights into the working of this rapacious parasite. Meanwhile, more than half a century after Brahmachari’s discovery of urea stibamine, scientists have finally managed to figure out its mode of action: the drug potently inhibits topoisomerase, the enzyme that unwinds the parasite DNA in order for it to be replicated. Although the anti-cancer Miltefosine and the anti-fungal Amphotericin B are the current drugs of choice against kala-azar, the insight into urea stibamine’s mode of action promises to usher in newer, more potent topoisomerase inhibitors. Fittingly, those spearheading this research are all Bengalis, toiling away in a laboratory a stone’s throw from what was once Brahmachari’s own.
Brahmachari, in one of his lectures, had remarked: “Today, Yellow Fever is on a retreat in the Americas. The same will one day be said of Kala azar, and it may be hoped that before long the disease will be completely banished from India and other parts of the world where it occurs. When the disease disappears from the world, then one of the highest trials of tropical medicine will be achieved.”
A hundred years on, that day is still awaited.
*****
Note: The authors are grateful to Dr Sudha Parashar for the generous gift of Sir Upendranath Brahmachari’s seminal book Gleanings From My Researches, Calcutta University Press, 1940.
Through this book, Brahmachari hoped “to infuse the spirit of research into the minds of students of medicine in India and not least amongst those whose paths are restricted to institutions where proper facilities for research are not yet available”.
This article first appeared in swarajya on Aug 19, 2017.